Fiona Jardine
Both the World Health Organization and the American Academy for Pediatrics recommend that babies should be exclusively breastfed for the first 6 months of life, so I, like the vast majority of parents, was determined to breastfeed my daughter after her birth in 2016. [1] Unfortunately, due to a variety of obstacles, my baby and I were not able to establish a direct nursing relationship. [2] Statistics show that my struggles are not unique: in the United States, 83% of babies receive at least one breastfeeding, but only 47% are exclusively breastfed at 3 months and 35% at 6 months. [3]
 My breastfeeding journey did not stop with a failed latch. While I was devastated that we would never have the “gold standard” of baby nutrition, bonding, and comfort, I was still determined to give her my milk any way I could. I knew vaguely how to express milk with a breast pump, but, despite having taken a breastfeeding class and having spoken at length about breastfeeding with our doula, I had little clue how to do it as the sole means of extraction. Online research on the topic didn’t help either, until, about two weeks postpartum, I finally discovered the term “exclusive pumping” (EP, EPing, EPer). Through social media, specifically Facebook groups, I learned how to sustainably EP, received answers to specific questions, and felt understanding and support for my situation. I am proud to say that my daughter was exclusively breastfed until we introduced solids.
My breastfeeding journey did not stop with a failed latch. While I was devastated that we would never have the “gold standard” of baby nutrition, bonding, and comfort, I was still determined to give her my milk any way I could. I knew vaguely how to express milk with a breast pump, but, despite having taken a breastfeeding class and having spoken at length about breastfeeding with our doula, I had little clue how to do it as the sole means of extraction. Online research on the topic didn’t help either, until, about two weeks postpartum, I finally discovered the term “exclusive pumping” (EP, EPing, EPer). Through social media, specifically Facebook groups, I learned how to sustainably EP, received answers to specific questions, and felt understanding and support for my situation. I am proud to say that my daughter was exclusively breastfed until we introduced solids.
Despite the vitally important health benefits of breastfeeding to both the breastfeeder and the recipients of human milk, as well as the increasing number of EPers, research on EPing is scant. The research that exists is often limited to analysis of the composition of expressed milk, pumping in the context of the neonatal intensive care unit, or secondary analysis of existing data. While there are some studies about milk expression more generally, I found no published research documenting the lived experiences of EPers specifically, including why they EP, where they find information, what support they get, how they eel, and problems they have. My field, Information Studies, encompasses a broad variety of topics—human–computer interaction, information management, library science, and archives, to name a few— and provides me with enough latitude to ask all of these questions (and more).
So ask I did. I explored this gap in research, at the same time collecting data on public health and lactation science issues such as formula feeding, milk supply, and postpartum health. My data collection involved a cross-sectional, self-report, mixed methods online survey. Between March 2017 and March 2018, I collected both qualitative and quantitative data through an initial survey, gathering over 2,000 qualifying responses. In addition, anyone currently EPing was given the option to participate in periodical follow-up surveys: so far, over 700 follow-up surveys have been completed by 341 respondents over a period of 18 months. While some PhD researchers struggle to collect enough data, I suffer from the opposite problem. The initial survey is long and has quite a few open-ended questions, yet respondents took their time (often over an hour) to share their experiences at length. This is a clear indication of how passionately EPers want their voices to be heard; many report that lactation/medical professionals dismiss EPing as a legitimate option.
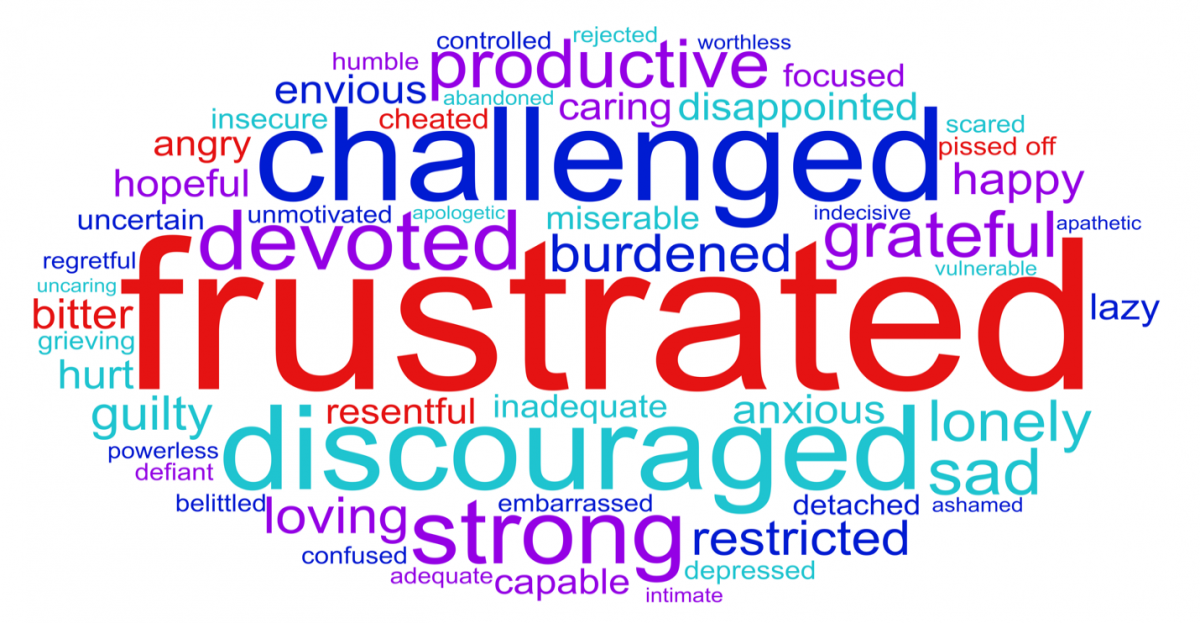 While data analysis is ongoing, I analyzed EPers’ prenatal information needs, seeking, and use in a paper for The Journal of Human Lactation. [4] For that paper, I also analyzed the feelings of EPers about EPing, which resulted in a pretty disheartening word cloud (from a list of 57 words, respondents were asked to pick all those that they had ever felt about EPing. In this weighted word cloud, the bigger the word, the greater number of respondents selected it).
While data analysis is ongoing, I analyzed EPers’ prenatal information needs, seeking, and use in a paper for The Journal of Human Lactation. [4] For that paper, I also analyzed the feelings of EPers about EPing, which resulted in a pretty disheartening word cloud (from a list of 57 words, respondents were asked to pick all those that they had ever felt about EPing. In this weighted word cloud, the bigger the word, the greater number of respondents selected it).
My most recent analysis has been to answer the question, “why do EPers exclusively pump?” Preliminary findings indicate that most (69%) respondents reported some sort of latch problem, 25% that their baby did not get enough milk while nursing, and 23% had an infant in the neonatal intensive care unit. Only 8% of respondents “just wanted to” EP.
While my study collected data on a wide range of topics, my dissertation will focus on the information behavior (that is, information needs, seeking, and use) and support needs of EPers. My research will identify the knowledge gaps of both lactating people and lactation care providers, as well as strategies to fill these gaps. The identification of these strategies is vital to creating evidence-based changes to both breastfeeding policy and practice, such as less focus on nursing and more support for feeding human milk no matter the method. I believe changes such as these will increase the incidence and duration of breastfeeding and therefore promote child and parental wellbeing, as well as improve the lived experiences of EPers and the practice of EPing more generally.
[1] World Health Organization. (2003). Global strategy for infant and young child feeding. Geneva: World Health Organization.
American Academy of Pediatrics. (2012). Policy statement: Breastfeeding and the use of human milk. Pediatrics, 129(3), e827–e841. http://doi.org/10.1542/peds.2011-3552.
[2] Direct nursing is when a child suckles and feeds at the breast, rather than eating from a bottle.
[3] With the exception of medication and vitamin D supplements, a baby only ingests human milk.
Centers for Disease Control and Prevention (2018). Breastfeeding Report Card 2018. Retrieved from https://www.cdc.gov/breastfeeding/data/reportcard.htm on September 7, 2018.
[4] Jardine, F.M. (2018). Breastfeeding without nursing: “If only I’d known more about exclusively pumping before giving birth.” Journal of Human Lactation. doi: 10.1177/0890334418784562.
About the Author:
 Fiona Jardine is a PhD candidate at the College of Information where she is conducting pioneering research into the experiences of those who exclusively pump human milk; follow along with her findings here: bit.ly/EPresearch. Fiona is also an Advanced Lactation Consultant and a postpartum doula so that she can provide the support that she believes is so desperately needed, especially in the fourth trimester. Find out more about Fiona on her website: fionamjardine.com.
Fiona Jardine is a PhD candidate at the College of Information where she is conducting pioneering research into the experiences of those who exclusively pump human milk; follow along with her findings here: bit.ly/EPresearch. Fiona is also an Advanced Lactation Consultant and a postpartum doula so that she can provide the support that she believes is so desperately needed, especially in the fourth trimester. Find out more about Fiona on her website: fionamjardine.com.